
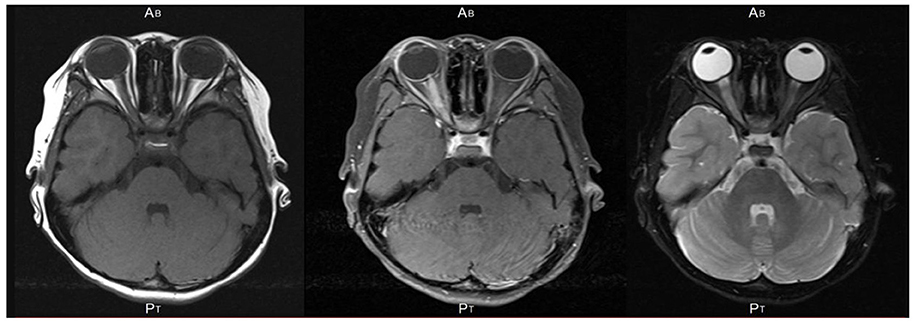
With evidence of increased intracranial pressure by LP findings, acetazolamide 250 mg TID was initiated. Lumbar puncture (LP) revealed an opening pressure of 45 cm H 2O, and 40 mL clear and colorless CSF was drained at this time. Magnetic resonance image (MRI) head and MR venogram (MRV) showed no intracranial abnormality, and venous system was well opacified without sinus venous thrombosis. Here, the patient was admitted to the inpatient medical ward with a clinical suspicion of idiopathic intracranial hypertension. CT head revealed slightly bulky left optic nerve with/without CT evidence of acute intracranial abnormality. COVID‐19 PCR was negative on current admission. Laboratories were only remarkable for microcytic anemia. Ophthalmology examination showed severe optic disk edema on the left and mild on the right side, color vision 1/7 in the left eye and 7/7 in the right. Initial vitals were normal with temperature of 36.8☌, respiratory rate of 19 breaths per minute, blood pressure of 145/80 mm Hg, oxygen saturation of 99%, and weight of 117.3 kg. This headache was followed by blurring of vision that worsened gradually over 1 week and difficulty distinguishing colors especially in the left eye as well as painful eye movements. In the 2‐week period, she started exhibiting gradually progressive holocephalic headache, described as pulsatile that awakens her from sleep, associated with nausea and importantly was different from here usual migraine episodes. Her past medical history was significant for diabetes mellitus, obstructive sleep apnea, migraine, gastritis, obesity, and a recent hospitalization for 10 days due to mild COVID‐19 and treated as our local guideline with azithromycin, hydroxychloroquine for 7 days, and amoxicillin‐clavulanic acid and discharged in good condition. 7, 8Ī 38‐year‐old female presented to the accident and emergency department in our hospital with history of headache and blurry vision. 3 Several cases have also documented the ability of SARS‐CoV‐2 virus in dysregulation of the immune system, with COVID‐19 cases presenting as Guillain‐Barré syndrome, 4 Miller Filler syndrome, 5 Kawasaki syndrome, 6 antiphospholipid antibody syndrome, 4 and anti‐MOG antibody‐induced optic neuritis. Recent reports have demonstrated the plausible neuro‐invasive potential of SARS‐CoV‐2 infection, 2 and it has also been hypothesized that SARS‐CoV‐1 may trigger autoantibody production. The first case of COVID‐19 emerged in Wuhan, China, in December 2019, 1 following which the surge in COVID‐19 cases reached a pandemic proportion by March 2020. Further experimental models and research are warranted to better understand how the acute and chronic course of illness in the context of SARS‐CoV‐2 could further modulate our approach and treatment. The accumulative number of reports of COVID‐19 patients with demyelinating manifestations such as bilateral optic neuritis with clinical and radiological features of NMOSD/anti‐MOG syndrome delineate that probable neuro‐invasion is a reasonable concern that SARS‐CoV‐2 is an emerging neuropathogen. To the best of our knowledge, this is the first case report to establish concurrent intracranial hypertension, seronegative neuromyelitis optica syndrome disorder (NMOSD), and SARS‐CoV‐2 infection. We report the case of a young obese lady, recently discharged after treatment for COVID‐19, who later presented with headache and blurred vision, diagnosed to have pseudotumor cerebri and concurrent bilateral optic neuritis. Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infections have presented with numerous neurological manifestations, providing insight into the potential of SARS‐CoV‐2 virus in triggering autoantibody production and dysregulating the immune system.


 0 kommentar(er)
0 kommentar(er)
